This is a contributed op-ed written by Heather Zenk, senior vice president at Strategic Global Sourcing. Opinions are the author's own.
If there was ever a moment that has proven the resilience of the pharmaceutical supply chain, it is now.
The world was not ready for COVID-19, the largest and most devastating pandemic in modern history. It has presented many challenges — both to the front lines of healthcare and the back end supply chain. But together, pharma manufacturers, hospitals, physician practices, pharmacies and distributors have adapted and evolved in real time.
What’s next? One of the most important responsibilities of a distributor is to help stabilize the supply chain.
With demand for specific products related to COVID-19 treatments soaring, distributors have had to adjust their approach to helping the industry manage inventory and ensure all sites of care have access to needed medications.
Typically, this work is done through allocation programs, but the impact of COVID-19 has caused many distributors to redesign what those programs look like. And while the supply chain has shown its resilience, distributors must prepare the healthcare and pharmaceutical supply chain for the unique considerations of a COVID-19 vaccine that is ready to enter the commercial market.
Allocation programs
Allocation programs are an important tool in helping to stabilize the supply chain. They ensure a single customer (such as pharmacy, health system, provider and others) can only order a fair amount of a designated product, so there is enough supply for as many sites of care as possible.
Distributors constantly monitor the marketplace for spikes in demand or dips in product availability and will place products on "allocation" if there is either a short supply or the potential for short supply.
Prior to COVID-19 and outside of an emergency, pharmaceutical distributors used a "fair share" allocation model. This approach helped ensure as much product as possible reached as many providers as possible across the country. It allowed customers to buy, for example, up to 125% of their historical purchase amount of a certain product.
Before the pandemic, using a standard, fair-share allocation methodology helped safeguard against any well-intentioned providers overstocking products and creating access issues for other sites.
One of the most important responsibilities of a distributor is to help stabilize the supply chain.

In the virus’s early days, AmerisourceBergen saw many products used to support COVID-19 cases — from sedatives, inhalers, antivirals and antipyretics to over-the-counter cough/cold medication and isopropyl alcohol — in short supply due to much higher than normal demand across the country. These products were still being produced at the same rate, if not faster.
But in some cases, it was not possible for manufacturers to keep up with such a sharp increase in demand.
For instance, in March, AmerisourceBergen saw unprecedented "surge ordering" across our distribution network as pharmacies, hospitals and health systems throughout the country placed orders at three to five times their historic purchase volumes — all at the same time.
Every provider, especially those in the acute-care setting, was looking to bolster inventory in response to, or anticipation of, a significant increase in patients admitted to the hospital.
This was particularly true for products like hydroxychloroquine, azithromycin, albuterol inhalers and injectable narcotics, where we were experiencing overall demand exceeding available supply. But, it also applied to other medications where patients were trying to fill longer-term scripts, knowing they needed to practice social distancing for the coming weeks.
In fact, at the beginning of the crisis — between March 12 and March 15 — we saw a nearly 50% surge in orders across our entire network, and went from distributing approximately 4 million products every day to nearly 6.5 million in just a matter of days.
COVID-19 created an unprecedented situation — with exponential growth in the number of patients occupying intensive care unit beds, more ICU beds added, and new "pop-up" hospitals erected for patient care — that would have been impossible for anyone to prepare for. The models that once proved effective needed to undergo an evolution.
An evolved model
The growing demand for products required distributors, and the supply chain as a whole, to be dynamic, ensuring as many healthcare providers across the continuum of care as possible received much needed medications. We had to shift our allocation procedures to respond more directly to the evolving situation and stabilize availability across heavily impacted points of care.
In addition to considering a provider’s previous purchase history, it was critical allocation methodologies appropriately factored in existing and emerging hot zones, analyzing, for example, the prevalence of COVID-19 patients and the number of ICU beds at a facility.
Stakeholders are now preparing for the next phase: bringing a vaccine to market.

In these situations, product needs were truly emergent and could not be based on historical demand. Communication became the bedrock of our efforts as we educated manufacturers on the scope of increased need, provided updates to critical sites of care, and bought as well as distributed in-demand inventory from manufacturers as soon as we had it in stock.
While we have seen more stabilization within the supply chain, stakeholders are now preparing for the next phase: bringing a vaccine to market.
Planning for a vaccine
It is estimated that the United States population, alone, will require more than 300 million vaccine dosages at the very least, making it all the more important that the full pharmaceutical supply chain prepare and collaborate, so that all sites of care that need and deserve access to this product receive it.
Since the federal government has supported many manufacturers and given them the funding necessary to jump start the development process of such a complex vaccine, the government will receive much of the initial supply. In addition, healthcare workers will be the first to receive the vaccine, followed by essential workers, those 65 years old and older, and high-risk individuals once supply is available. We likely won’t have substantial supply until mid-2021 and commercial availability until late-2021.
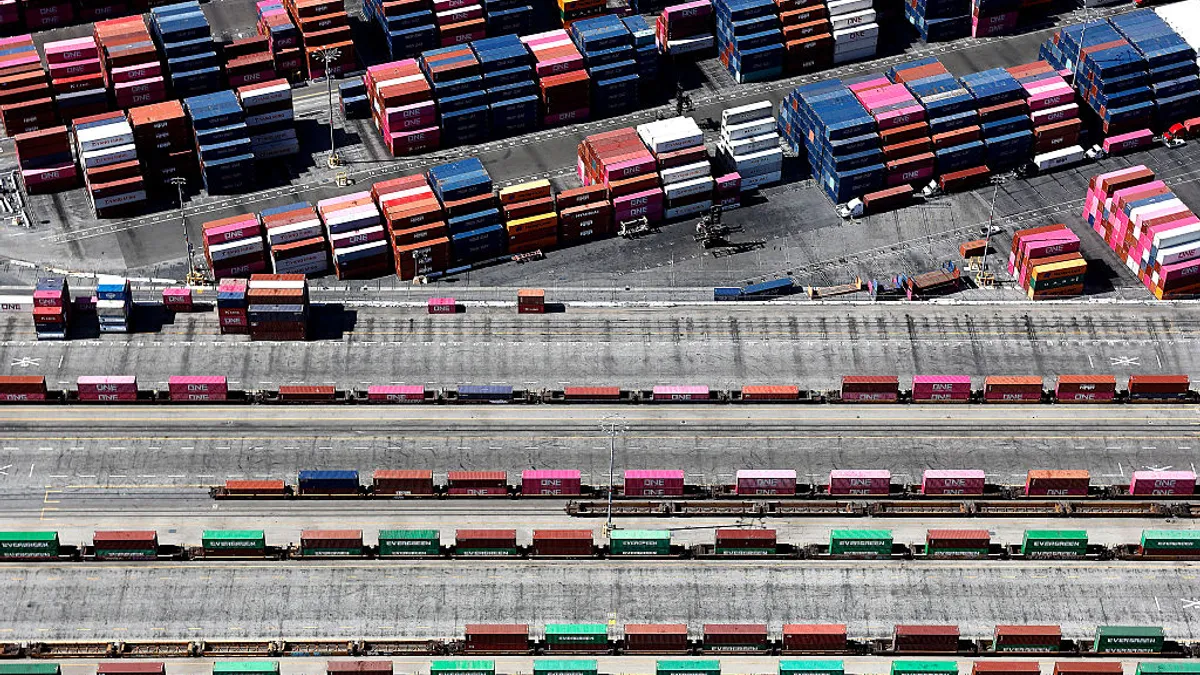
As the industry looks toward a vaccine and bridging from clinical trials or the initial government allotment and then on to the commercial market, manufacturers must be ready to scale operations in order to reach all providers that will be responsible for administering a vaccine, which could include 230,000-plus physician practices, 1,200 health clinics and 6,000-plus hospitals and other channels, like the U.S.’ 90,000 pharmacies.
For a vaccine to truly be accessible to all patients, pharmacies should ultimately be a site of care for administration. Pharmacists critical role is evident by the Department of Health and Human Services’ recent authorization of pharmacists to order/administer COVID-19 vaccinations (once available) to persons age 3 and older.
With nearly 90,000 pharmacies in the United States, they are some of the most accessible healthcare destinations in this country, especially in rural areas, which may be difficult to otherwise reach.
We likely won’t have substantial supply until mid-2021 and commercial availability until late-2021.

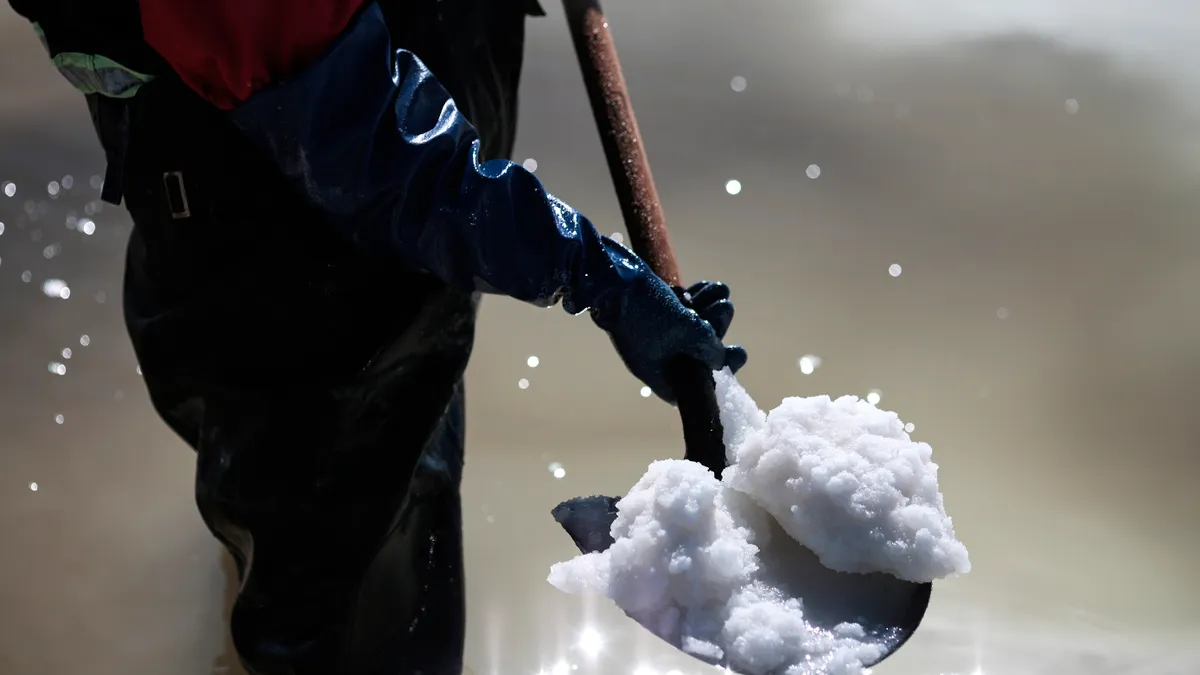
Regulators, manufacturers, distributors and sites of administration will also need to work together to support a vaccine’s unique product requirements at scale. For instance, it is expected that a COVID-19 vaccine may require frozen (minus 20 C) or deep frozen (minus 70 C) transport and storage, something high-demand products have never previously needed.
With the FDA’s decision to provide certain COVID-19 product approval via its emergency use authorization authority, there are also packaging and labeling requirements that differ from a traditional approval process. These requirements will necessitate conversations across the supply chain, so all parties are in sync. Failure to do so may risk product viability and as a result, patient success.
No matter how the COVID-19 pandemic or the development of the vaccine evolves, manufacturers and providers can trust and rely upon their wholesale distributor partner to responsibly get medicines to the people who need them the most.
Distributors are constantly evaluating allocation methodology to understand where demand for products has fallen and adjusting based on real-time information while taking a human-focused lens to build out new business continuity plans that prepare for the next widespread challenge to the supply chain.
Distributors are the lynchpin to successfully navigating and securing the pharmaceutical supply chain. By collaborating across the supply chain, the pharmaceutical industry can be instrumental in unlocking the curative potential that a COVID-19 vaccine could offer to patients around the world. Together, we can all keep the supply chain secure, yet nimble — resilient and responsive for patients everywhere.
This story was first published in our weekly newsletter, Supply Chain Dive: Procurement. Sign up here.