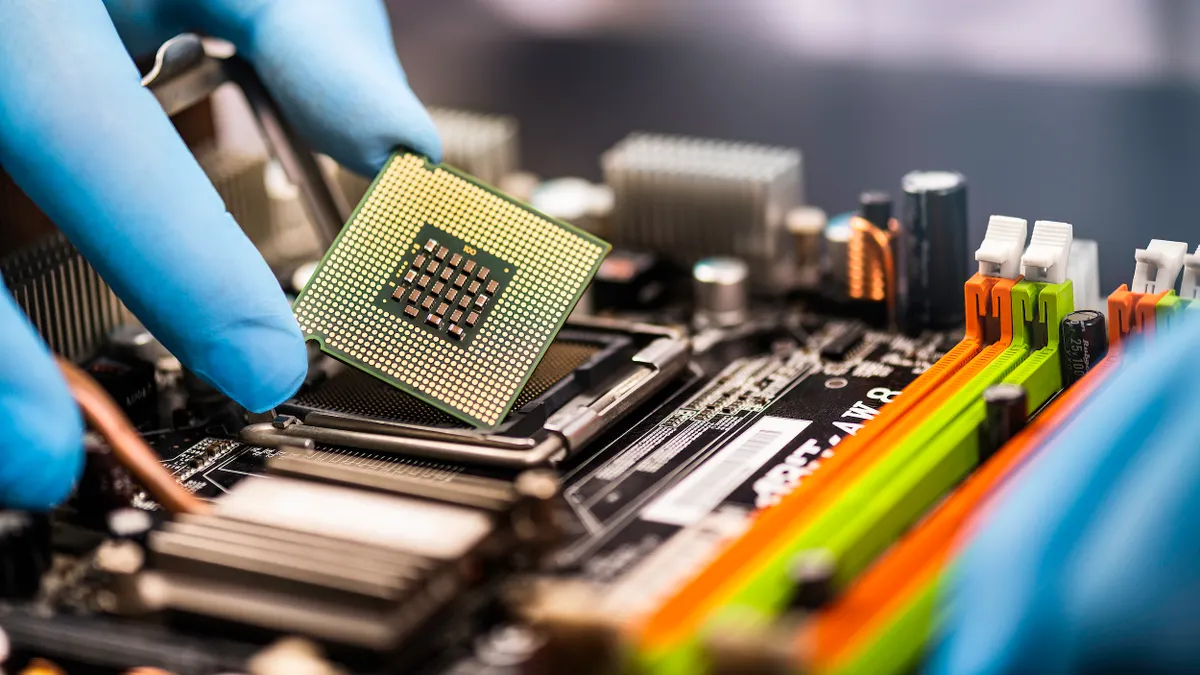
A decade-long regulatory deadline is looming for the pharmaceutical supply chain to electronically share drug data from end-to-end, or risk healthcare ecosystem instability.
Come Nov. 27, if a pharmaceutical manufacturer can’t provide unit-level serialized products to its distributors, no one along the supply chain can legally move it to the next step. If the distributor is unable to provide the pharmacy with electronic tracing data, the pharmacy can’t legally receive the product, let alone dispense it to the patient.
The new rules come as a result of the final implementation stage of the Drug Supply Chain Security Act, known to the industry as DSCSA, which aims to facilitate drug traceability and help ensure patient safety. Companies have been preparing to comply with the law’s various milestones for some time, as it was enacted nearly a decade ago.
But as the final compliance step approaches, association surveys and public meetings alike show stakeholders fear technical or practical unreadiness could throw a wrench into the drug supply chain.
Industry voices raise concerns over readiness
A supply chain is only as strong as its weakest link, and pharmaceuticals depend on many actors along the way to ensure drugs get to consumers.
Manufacturers, repackagers, wholesale distributors, third-party logistics providers, and drug dispensers like hospital and retail pharmacies must all comply with new requirements under the DSCSA. While many companies say they are fully prepared, Elizabeth Gallenagh, general counsel and senior vice president of supply chain integrity at the Healthcare Distribution Alliance, said there are still gaps along the chain.
Gallenagh said part of the issue with industry readiness is that many companies are treating Nov. 27 as a prompt for action, but data problems could result from a lack of prior testing.
“In their mind the compliance date is their trigger,” Gallenagh said. “This is the flaw in the law. The last push has been written as flipping the switch, but you can’t flip the switch and have it work seamlessly.”
Collaboration, technical issues lead list of challenges to meeting DSCSA
Gallenagh said she has heard reports that less than half of manufacturers are currently ready to share data with distributors as well as concerns from dispensers about whether they can provide products to patients if they don't have the right data once the DSCSA is enacted.
Gurdeep Sidhu, manager of QA global policy at Canadian generics manufacturer Apotex, said there are also challenges with the downstream connectivity.
“Not all the partners are on board with the requirements," Sidhu said in a December public meeting on implementation challenges, hosted by the Food and Drug Administration. "We want to make sure that there are some exceptions outlined, and how do we handle them.”
What if companies can’t share data?
As of Nov. 27, if any link along the supply chain is not able to receive and transmit the tracing information electronically, the drug cannot move to its next step.
“Technically distributors can’t receive or sell product downstream if they haven’t received the appropriate data from the manufacturer,” Gallenagh said. “If you don’t receive something, you can’t send something.”
The Healthcare Distribution Alliance is concerned about a product stoppage and is requesting a “stabilization” period from the FDA to allow the product to flow and continue moving toward the unit level traceability goal. It could involve narrow exemptions and some delays for specific requirements.
"You can’t flip the switch and have it work seamlessly."

Elizabeth Gallenagh
General counsel and senior vice president of supply chain integrity, Healthcare Distribution Alliance
The FDA also received feedback from other stakeholders on their level of readiness and implementation challenges at the FDA’s public meeting in December.
The regulator said in an email to Supply Chain Dive that it plans to finalize several draft guidelines by November, including the standards for data exchange. The FDA also said it heard concerns from stakeholders about small entity compliance efforts, including small dispensers with 25 or fewer employees, and will continue investigating whether alternative methods for compliance are needed.
“FDA will be conducting a small dispenser assessment that will examine necessary software and hardware’s accessibility, cost to obtain, install, and maintain, and integration into business practices,” the spokesperson said, noting the study will inform potential alternate compliance methods. “Continued outreach is needed because stakeholders felt there is still a lack of understanding of the complexities and needs to meet DSCSA requirements, particularly small entities.”
On May 11, the FDA agency announced the process for stakeholders to request a waiver, exception or exemption from the act’s requirements. It has already exempted some COVID-19 products.
As for compliance, Gallenagh said enforcement of the DSCSA may be relegated to different actors, such as the FDA for manufacturers and state authorities for pharmacies. But if there is strict interpretation and enforcement of every aspect of the law by the end of November, there will be product shortages.
“The wiser person says there’s no way they can let that happen,” Gallenagh said. “It’s safe to say, everything will not be perfect on November 27.”