Dive Brief:
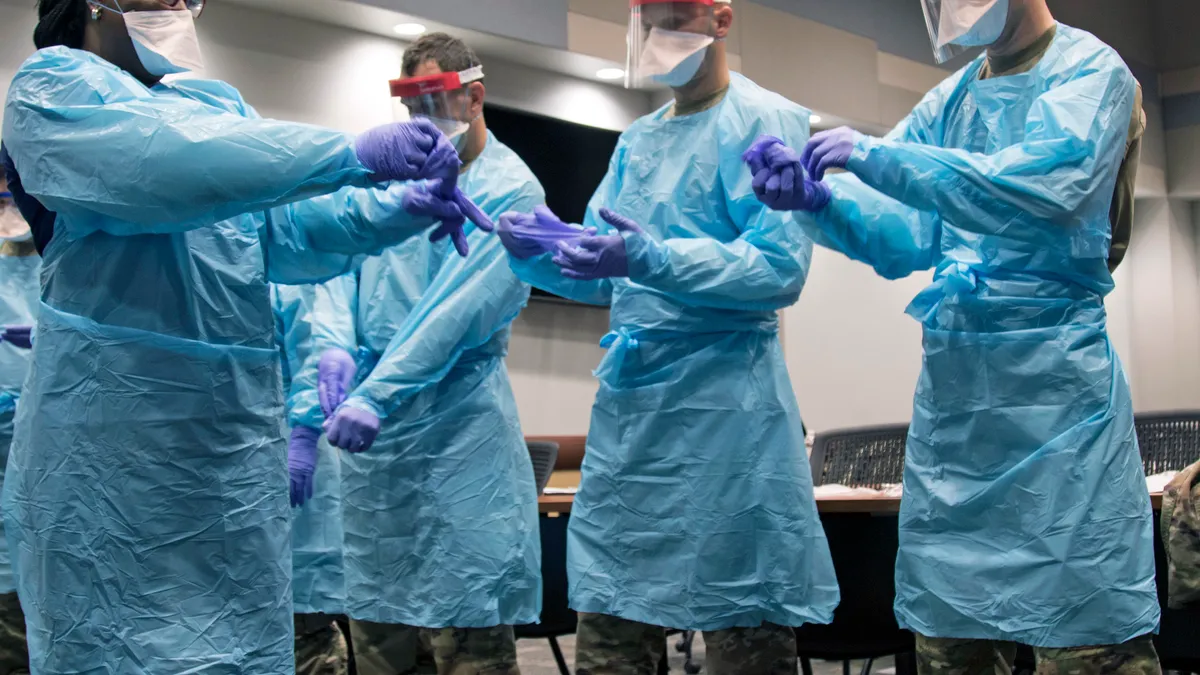
- Supply chains are struggling to build personal protective equipment inventory, with 77% of respondents saying they have no supply remaining for one of more types of PPE, according to Get Us PPE's August shortage index. Get Us PPE is a nonprofit that distributes PPE donations. The index, which the nonprofit says is the largest of its kind, is based on a database of requests the organization receives.
- "While large hospital systems are beginning to benefit from a recovering PPE supply chain, smaller, non-hospital facilities are still facing acute PPE shortages," Get Us PPE said in a report accompanying the survey.
- The three most requested items in Get Us PPE's database in August were N95 respirators, disinfecting wipes and surgical masks, the organization said.

Dive Insight:
PPE manufacturers acknowledge the ongoing issue of availability and stock.
"3M is making and distributing more respirators than ever before, though demand continues to far outpace what the entire industry can supply," 3M CEO Michael Roman told analysts at the end of July.
It is especially difficult to obtain PPE in rural parts of the country because of the geographic location, the cost of ordering PPE in small amounts and the inability of smaller organizations to meet minimum order quantity, according to Alizée Weber, the deputy director of operations at Get Us PPE.
Some organizations have turned to cleaning and sanitizing used PPE to help extend the life of its existing inventory. And they're relying more on homemade alternatives, she said.
Healthcare providers are also making changes to procurement practices to try to get the PPE they need. Some are moving to multi-source contracts instead of single-source contracts, Association for Health Care Resource & Materials Management Senior Director of Supply Chain Mike Schiller said in an emailed statement. Others have turned to group purchasing.
"The supply chain remains fragile and overtaxed by the worldwide demand for PPE," Schiller said.
Get Us PPE manages its donation inventory without a centralized warehouse or storage location and relies on organizing logistics between the donator and requestor, Weber said.
"We've really strayed away from ... having a warehouse just because I think it was so time-sensitive to get the PPE to where it was needed," she said, adding that the donor will often handle shipping. It typically takes one to two weeks for donations to move from a donor to a requestor.
While survey results show that shortages have been persistent for the last four months, there have been changes in who is looking for PPE through Get Us PPE's database. The organization started out as a way for individuals to donate PPE to other individuals or healthcare facilities.
In April, hospitals accounted for 47% of requests compared to 53% of requests that came from non-hospital groups like homeless shelters, dental clinics, nursing homes or social services. By August, hospitals accounted for 10% of requests, partly because Get Us PPE had opened up to requests from schools, hurricane shelters and more social service organizations since it originally launched.
It is also now receiving more donations from manufacturers and corporate partners rather than individuals, Weber said. But even with more stock coming from larger suppliers, more than three quarters of requesters have no PPE inventory remaining.
"The supply of N-95s continue to remain a concern, and while the supply of gloves and gowns has improved, given how often practitioners use a new pair or gown for each patient, their supply is always a concern," Schiller said. "As states mandate PPE stockpiling, N95 manufacturers in particular will be forced to chase ever-increasing demand which will further strain this scarce commodity."
Get Us PPE has gotten requests for 21 million units of PPE total. It has been able to fulfill about 10% of those requests.
"This is really an indication of how severe the crisis is," Weber said. "I know a lot of people are eager to put this behind us. But the crisis is still very much going on."
This story was first published in our weekly newsletter, Supply Chain Dive: Operations. Sign up here.