Growing shortages of medical supplies at U.S. hospitals indicate there’s much room for improvement in the supply chain. Even when inventory does meet demand, many facilities are counting, ordering and replenishing their supplies in a manner that is, at best, inefficient and costly.
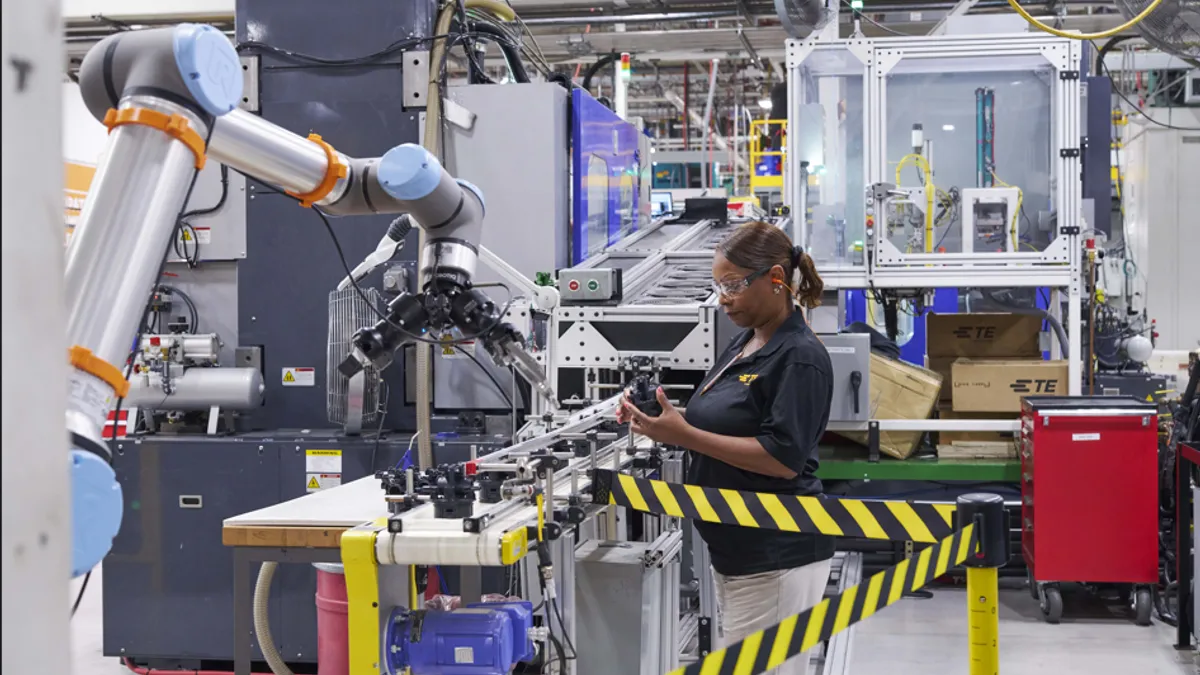
Experts says automating hospital supply chains can offer greater visibility, more accurate forecasting, and a means to help reduce costs throughout the healthcare continuum. Automation can reduce the need for clinical workers to engage in non-patient work and can help administrators make better long-term planning decisions.
Too many manual processes to manage thousands of SKUs
Several U.S. hospitals faced shortages of medical supplies in the Fall of 2017 after Hurricane Maria struck Puerto Rico and temporarily shuttered some of the island’s 80 medical device and pharmaceutical manufacturing facilities.
The shortages weren’t too surprising given many healthcare facilities lag behind the times in supply chain technology. A 2015 survey by Cardinal Health found that 18% of respondents had heard of a patient being harmed due to a lack of supplies.
Yet even when patient demands are being met, many healthcare facility supply chains can be inefficient and wasteful. A time and motion study by Cardinal Health of the Heart and Vascular Center at Adventists Health White Memorial in Los Angeles found the team was burdened by a manual, time-consuming process of ordering, replenishing and storing an inventory of 1,700 SKUs. It also had no easy way to track recalled products, little supply chain visibility and inconsistent workflows.
We reduced our inventory levels by knowing where things were.

Daniel Moreno
Cardiovascular Service Line Administrator, White Memorial Medical Center
Daniel Moreno, Cardiovascular Service Line Administrator at White Memorial Medical Center in Claremont, Calif. says the original inventory solution required staff to push a button every time they took something. And few were doing it in emergency situations.
“You’re not focusing on counting widgets, you’re there to take care of patients … Most people in the lab are clinical folks; that’s the last thing on their priority list,” Moreno says.
At the time, Moreno estimated the facility was expiring up to $15,000 of inventory per month. The operating room buyer was also buying for the Cath lab, and in busy times, supplies weren’t always ordered. Staff had to use multiple work-arounds to obtain supplies in what was a “ridiculous” process, Moreno says.
Simplifying processes and counts with automation
White Memorial Medical Center is not alone, as many hospitals lag the technology to optimize their medical supply chains.
Emergencies can make it difficult to predict what will be needed, so many faciliites opt to have too much on hand, rather than too little. As many facilities don’t have a clear view into on-hand inventory or forecasted demand, they have little ability to engage in effective planning.
“The golden nugget is the data to make proactive informed decisions,” says Tapan Shah, Director of Product Management at Cardinal Health. “There’s a patient safety issue, a liability issue. And it’s time-consuming to do basic inventory, even with a barcode solution.”
White Memorial implemented the Cardinal Health RFID Solution which helped automate hospital supply chain processes and deliver real-time end-to-end inventory visibility. Cardinal tagged all the products with RFID put them in smart cabinets that conduct counts every 30 minutes, then worked through processes while considering time management and what was and wasn’t on the shelf.
The golden nugget is the data to make proactive informed decisions

Tapan Shah
Director of Product Management, Cardinal Health
Within three months of adoption, the cardiovascular department saw a 67% reduction in the time staff spent manually counting supplies, reducing counts from months to minutes. It also experienced an 84% improvement in time spent placing orders and a 95% improvement in tracking expired products.
The first post-deployment inventory count matched exactly what it did and provided a huge time and cost savings. The hospital discovered they gave away at least $45,000 in supplies in emergencies because there was no charge code, Moreno says. Adventists Health White Memorial has also been able to consolidate processes and centralize inventory systems by knowing exactly where everything is. Whereas they previously had to run around and “look through thousands of products to find what you did or didn’t have,” it has now been refined into one streamlined process.
“There were huge cost savings. And as we went through the first six months, our inventory dropped. We reduced our inventory levels by knowing where things were,” Moreno says.
Improving inventory and healthcare with RFID
With automation offering more visibility into the supply chain, administrators can better estimate inventory levels and ensure more accurate billing of patients. RFID and automation can also put all inventory into one registry, increasing the interoperability of interfaces and reducing redundant data entry and processes, says Shah.
“The technology helps with some of the automation and interoperability of those interfaces which takes away all these steps around double or triple documenting something," he says. "We make it easy to document one place at one registry.”
While many larger facilities are already automating parts of their supply chain, most smaller institutions are lagging. It’s especially a concern as many of these institutions move to value-based healthcare models. Some hospitals still use RNs and clinicians to work overtime to conduct manual inventory counts, something that’s a “waste of their valuable time on a trivial task,” Shah says. And without the technology in place, staff members often do things their own way which can lead to inconsistent workflows and further errors.
While overstocks can be a cost burden, understocks can hamper patient care and have a ripple effect throughout the organization. That could lead to case cancellations, case delays and critical patient safety issues. “You can’t put a price tag on a patient coming back and suing your because you had an expired product going in there,” Shah says.