When the COVID-19 pandemic started, Trinity Health, like other healthcare organizations, went into high gear sourcing additional personal protective equipment for the hospitals and thousands of nonacute care organizations participating in its supply chain program.
Procuring enough supplies for the Michigan-based organization with 92 hospitals in 22 states was challenging.
"It was a lot of work, a lot of vetting of previously unknown suppliers," said Ed Hisscock, senior vice president of supply chain. It did not use distributors to get products, which arrived by the container to its Fort Wayne, Indiana, distribution center.
A year later, "we’re keeping up, but it’s a daily task for our sourcing team," Hisscock said. The system is currently well stocked with PPE such as masks and isolation gowns, maintaining 120 days of stock of everything but nitrile gloves and syringes. Those are currently at 50 to 70 days of inventory.
Indiana University Health is also operating with a strong supply, a six month reserve. "We’re at good place right now. Three or four SKUs out of 4,000 are hard to get, but that’s not bad at all," said Derrick L. Williams, executive director of logistics.
"We’re keeping up, but it’s a daily task for our sourcing team."

Ed Hisscock
Senior vice president of supply chain for Trinity Health
Prior to the pandemic, IU Health kept six weeks of supplies, raised to eight weeks during flu season.
After the Defense Production Act was enacted, 3M could supply IU Health with enough respirators, even if they weren’t the exact ones requested. Williams said IU Health used 200 to 300 masks a day prior to COVID-19, and is now consistently using 1,000 to 1,300 per day. It spiked at around 3,000 a day at the health system's peak, around late November.
But that doesn’t mean the entire country is flush with PPE. As COVID-19 enters its second year, the PPE procurement crisis continues wrecking havoc. The U.S. PPE situation is in better shape than a year ago, but the needs are greater as well. Testing and vaccination require ongoing supplies, as do nonacute care facilities – such as doctors and dentist offices – schools, daycares and prisons.
Most organizations requesting PPE have no remaining supply
"You would not be surprised to hear it’s the case of the haves and the have nots," said Michael Alkire, president of Premier, a healthcare group purchasing and supply chain organization. Aside from nitrile gloves, large systems have a significant amount of inventory, he said.
And the have nots? Get Us PPE, a nonprofit launched during the pandemic to provide free protective supplies to healthcare and essential workers, saw requests rise 260% between November and December, and another 48% from December to January. PPE requests from hospitals increased more than tenfold between December and January.
When the organization started in March, PPE donors gave in smaller quantities, like giving 50 respirators stashed in their garage, said Ram Bala, a professor of supply chain management and business analytics at Santa Clara University and a Get Us PPE advisory board member. Now the donations come mostly from larger businesses, providing respirators by the pallet.
Even with a greater supply, some healthcare organizations are still operating under the PPE usage restrictions. A survey conducted Oct. 22 to Nov. 5 by the Association for Professionals in Infection Control and Epidemiology found that 73% of respondents said their facilities required them to reuse respirators.
"You would not be surprised to hear it's the case of the haves and the have nots."

Michael Alkire
President of Premier
"Before the pandemic, not throwing an N95 mask away between patients would get a nurse fired," said Bonnie Castillo, RN, executive director of the California Nurses Association and National Nurses United during a Jan. 21 California congressional delegation briefing.
She said some nurses are being told to wear the respirator during their entire 12-hour shift, some are given incorrectly sized respirators which don’t provide a proper seal, and some are told to wear the same one when alternately seeing patients with and without a COVID-19 diagnosis, which can increase the risk of spreading the disease.
Of the facilities reporting a need for N95s to Get Us PPE in January, 86% said they are using the respirators at unsafe rates.
Some reprieve may come as mask prices are decreasing, but their usage will not return to pre-pandemic levels, and a secure supply isn’t guaranteed, said Alkire.
Millions of pairs of gloves
A worldwide shortage of nitrile gloves has many in procurement worried. Get us PPE reported double the requests for nitrile gloves in December, compared to November.
"Trinity burns through a million pairs of gloves a day," Hisscock said. While the health system has kept up with its needs, it is conserving in part by giving vaccine clinics vinyl gloves to use instead.
Gloves are not required for vaccine administration, but providers are more comfortable using them. Glove demand increased 40% since COVID-19 vaccination started, according to Premier data, and the average lead time to receive gloves is 35 days.
Premier said gloves have been backordered for months, and even after implementing conservation protocols, they’re still one of the top supply chain challenges. The raw materials for nitrile gloves are in short supply, as are the ceramic molds to produce the gloves. In addition, Top Glove, the largest global nitrile glove producer, shut down 28 factories in November due to a COVID-19 outbreak in its staff.
The most requested items at Get Us PPE in December 2020
| Rank | Type of personal protective equipment |
|---|---|
| 1 | Disinfecting wipes |
| 2 | Nitrile gloves |
| 3 | Hand sanitizer |
Source: Get Us PPE
Thermo Fisher Scientific told customers in November, "our suppliers have advised us that they cannot guarantee product availability or pricing due to global raw material shortages and supply chain constraints." Fisher Scientific canceled open orders mid-December, raised prices and reintroduced the SKUs a few weeks later, with the ability to cancel open orders at any time and no contracted discounts.
Some help is coming. A U.S. nitrile glove manufacturer is tripling capacity and will produce 800 million gloves annually and expand to producing 1.2 billion gloves per year by 2022. The Federal Emergency Management Agency extended a temporary final rule designating some scarce medical resources like N95 respirators, surgical masks, nitrile gloves, some hypodermic needles and syringes, and some surgical or isolation gowns exclusively for domestic use during the pandemic, through June 30.
While not PPE, hypodermic needles, COVID-19 testing kits, and cleaning wipes are still in short supply. Pfizer gained an emergency use authorization to extract an additional dose out of the vaccine vials, but there aren’t enough needles in the kit for that extra administration.
Allocating PPE equitably with data
Organizations like Premier and Get Us PPE are using big data to ensure PPE gets to the right place. Early in the pandemic, Premier repurposed one of its technology solutions using machine learning to anticipate disease surges by ZIP code based on hospital information. "We didn’t have the mass testing back then," Alkire said.
Premier is now using that system to determine PPE needs and dynamically allocate products. The analysis includes individual healthcare providers’ product days on hand, average daily use, average lead time to acquire PPE and the percentage of orders that were past due.
Get Us PPE developed a Fair Distribution algorithm to match donations with needs in an equitable fashion. Determining factors for matching include facility type, immediacy of need, medical staff’s risk of exposure, the local healthcare capacity and the vulnerability of those served by the requesting organization.

"It’s an Uber-like solution where we’re matching the donor with the recipient," said Bala, who created the algorithm. The system works to minimize transportation distance, since transportation is often donated too. It ensures the recipient can use the entire supply available, so none is wasted.
"There hasn’t been a very centralized mechanism of allocation by the federal government, and it’s been very competitive. It’s an economic issue," Bala said.
This summer, the American Medical Association reported that its members spent on average 57% more on PPE. Organizations requesting supplies from Get Us PPE often don’t have the budget to buy what they need, especially as prices have risen.
Prices are starting to come down, said Hisscock, though they’re not back to pre-pandemic levels. "Some of the routine competition is settling into the market. I suspect it will go even lower," he said.
"We definitely blew our budget."

Derrick L. Williams
Executive director of logistics at Indiana University Health
Williams still sees price gouging on items not covered by the DPA, from pop-up vendors. IU Health recently tried to order a canister of wipes that traditionally sold for $3 to $4, but was priced at $16.
IU Health used to pay 4 cents per surgical mask. At the pricing peak, it paid 50 cents to $1. "We definitely blew our budget," Williams said.
Get US PPE said N95 prices went up as high as $7 per mask, compared to pre-pandemic prices of 11 cents to 38 cents.
Masks are down to 8 to 9 cents, and 3M’s N95 masks are back to normal pricing, Williams said.
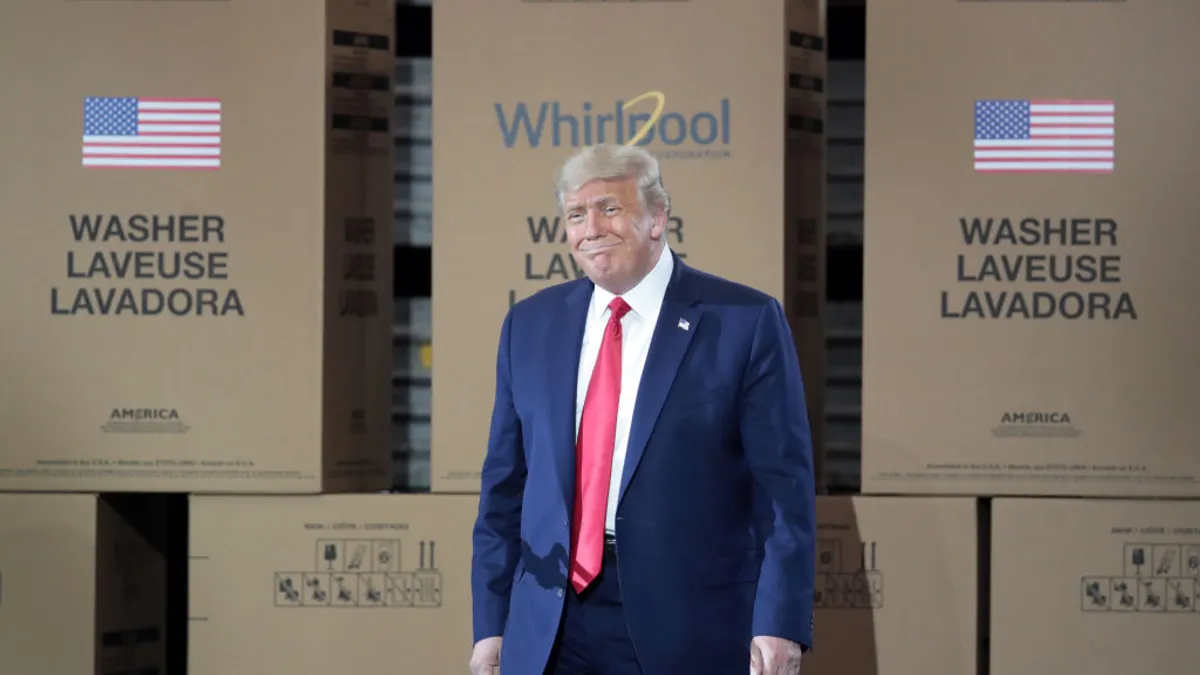
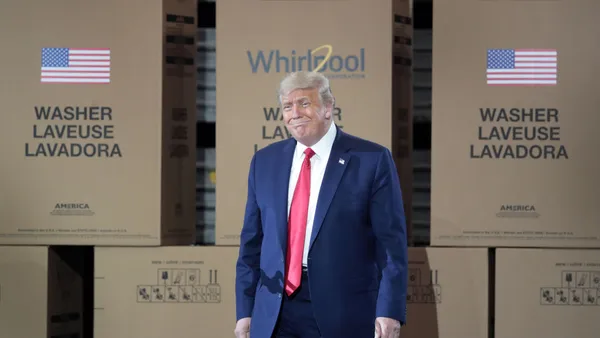
Standing up production stateside
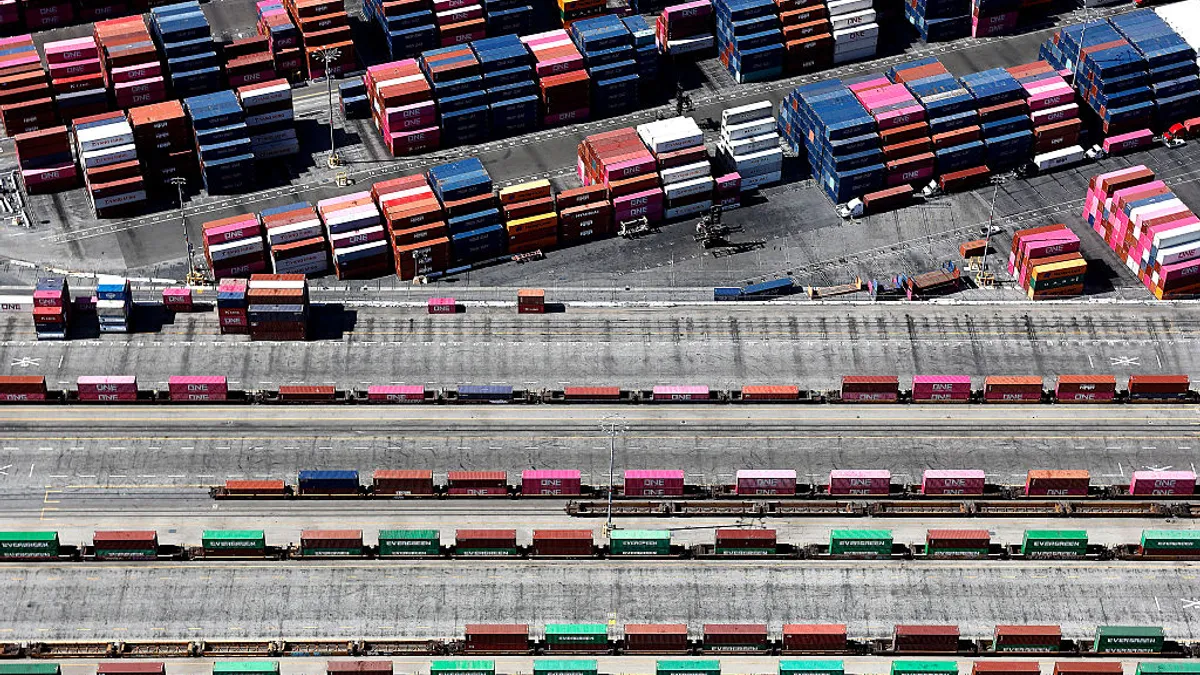
Most PPE is coming via container ship now, taking 90 to 120 days."We just don’t have the same urgency as at the height of the pandemic. We’re ahead of it now," Hisscock said, so air transport isn’t necessary. But ongoing container shortages are one reason Trinity Health wants to keep 120 days of stock in reserve, "because of the time it takes to get products."
Many organizations are stockpiling to guarantee supply. Hisscock is hearing about some organizations buying a year’s worth of PPE items.
"I get concerned about the waste when it starts to expire," he said, and that includes government supplies. He’s advocating with Michigan and federal governments to cycle PPE products through government emergency stockpiles to keep the stock fresh, sending a certain amount out to organizations on a regular basis and backfilling products in storage.
"From a supply chain perspective, we still have an incredible overreliance on China. I don’t think you can understate that."

Michael Alkire
President of Premier
Given the long lead times and high freight rates, many hospitals relied on domestic manufacturing to get to a greater PPE supply.
Almost a dozen manufacturers produced face shields, cloth masks, and hand sanitizer for Trinity Health. That included breweries making hand sanitizer, and a Ford Motor Company subcontractor making face shields.
"You don’t typically see the Ford Motor Company logo stamped on boxes of medical supplies," Hisscock said. Trinity received "very little viable product from state or national stockpiles," he said; some were expired PPE products.
As a result of the pandemic, IU Health increased domestic contracting. "I’ve done more business with local vendors since the pandemic, than in the previous five years I’ve been at IU Health. I think that strategy will grow," reducing the risks of procuring overseas, he said.
Premier and 16 healthcare systems invested in Prestige Ameritech to manufacture more N95 masks, and subsequently Premier and 34 health systems invested in DeRoyal to stand up isolation gown production. Both investments are for short- and long-term production.
While manufacturing increased domestically, "from a supply chain perspective, we still have an incredible overreliance on China. I don’t think you can understate that," said Alkire. That includes the raw materials.
Given the labor cost imbalance between the U.S. and southeast Asia, "it doesn’t make sense to stand up production [domestically] unless it’s a vital product, as it can be done more efficiently in a lower labor cost country," Alkire said.
Isolation gown manufacturing can be automated. "There’s a very low labor component," Alkire said. "We believe the price for that product will be globally competitive, because it’s highly automated."
This story was first published in our weekly newsletter, Supply Chain Dive: Procurement. Sign up here.